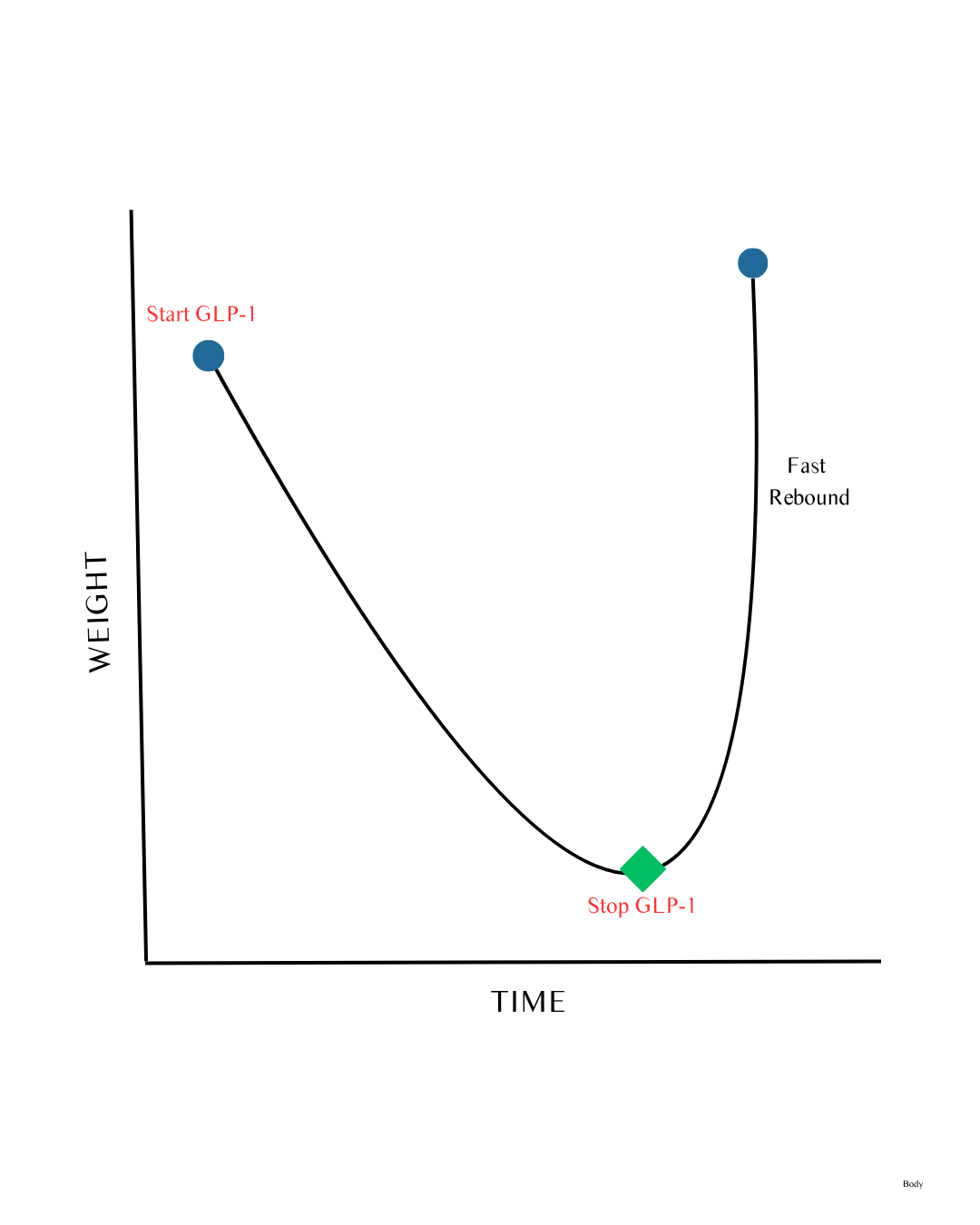
GLP-1 Is Not a “Weight Loss Switch”
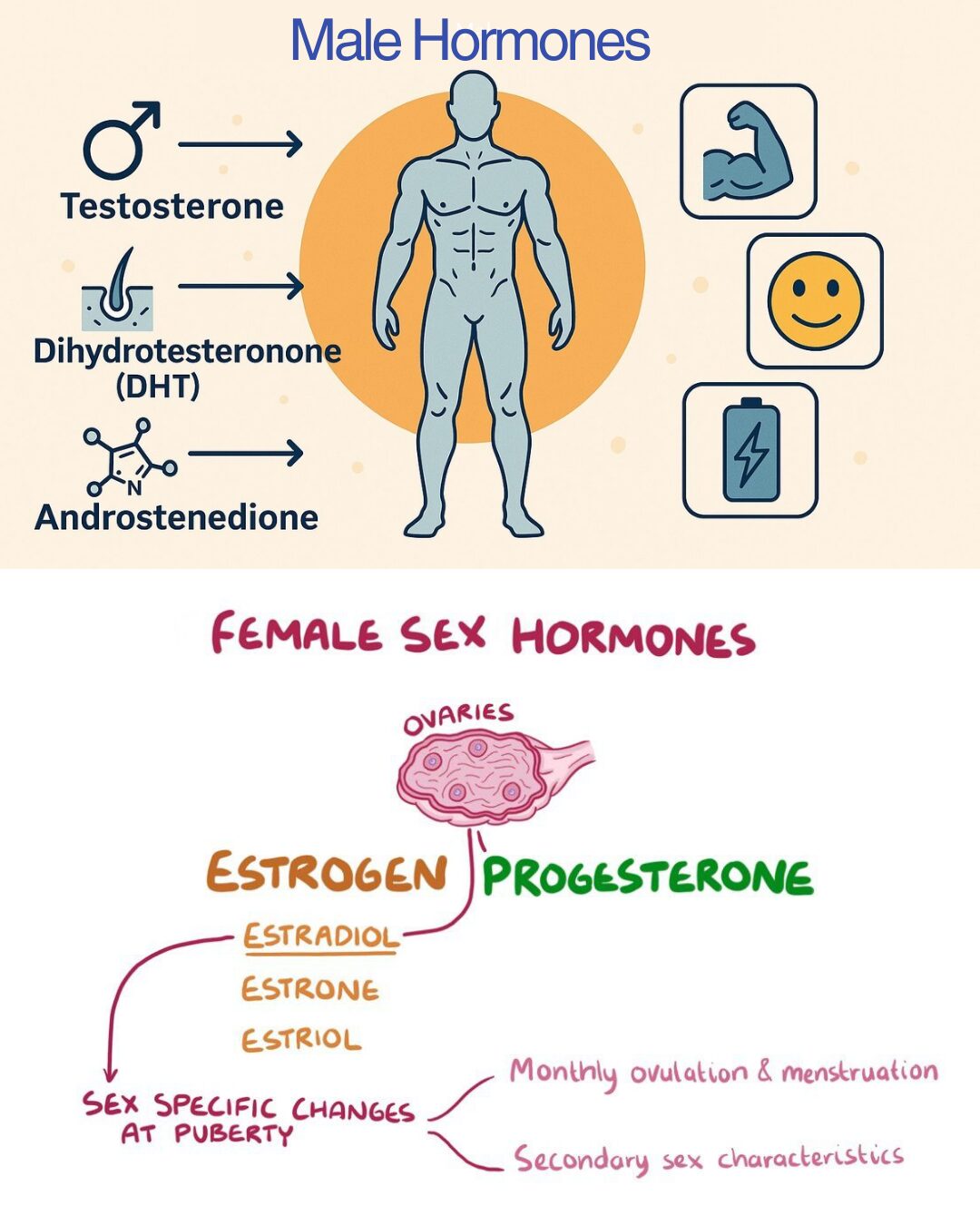
GLP-1 is a natural hormone your body already uses to coordinate:
- Appetite
- Digestion
- Insulin release
- Brain reward signals
- Stress responses
- Heart and kidney function
It’s not a single lever.
It’s a network signal.
When we amplify GLP-1 continuously with medication, we are not “fixing” one issue — we are commanding multiple systems at once.
Biology tolerates this briefly.
It never ignores it.